PANCREATIC SURGERIES
Pancreatic surgeries are highly complex surgeries. They are mostly performed in cases of cancers of pancreas, lower bile duct or duodenum, long standing, recurrent or persistent infections in the pancreas or their complications.
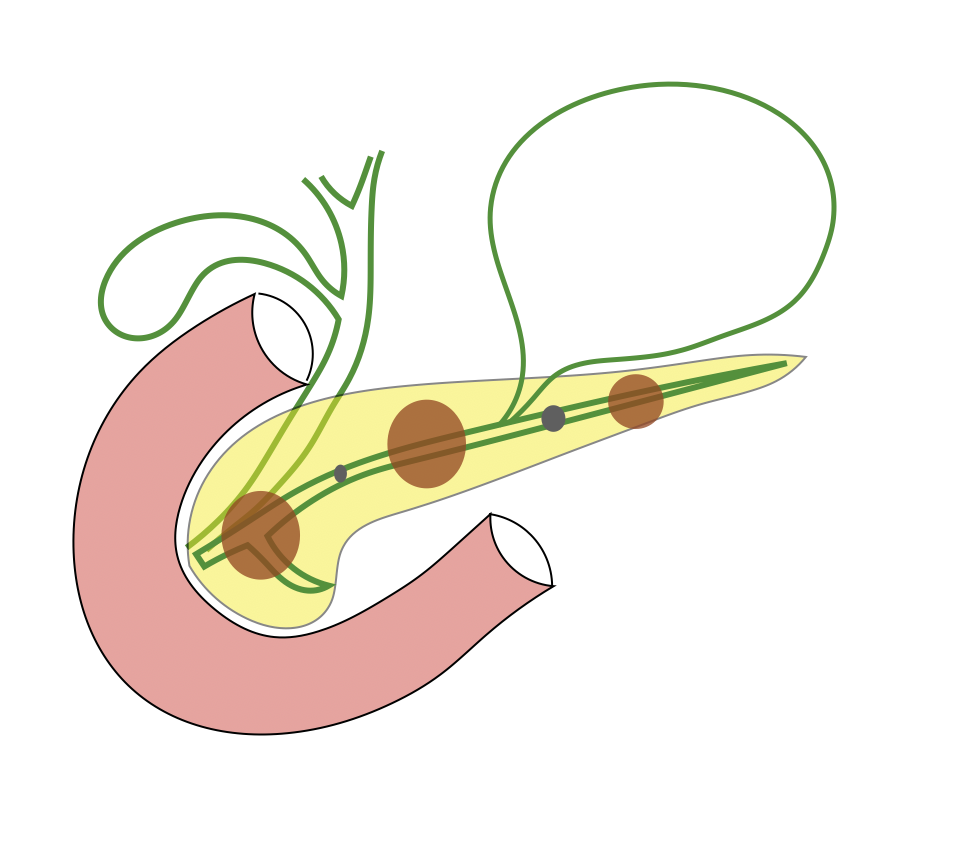
Depending upon the type of problem pancreatic surgeries can involve either removal or part of pancreas with or without surrounding structures like bile duct, duodenum or spleen, or drainage of obstructed pancreatic ducts or abnormal collections (Pseudocyst) around pancreas developing as complications of pancreatic infections.
A. Pancreatic Resection (Pancreatectomy): Depending upon the part of pancreas removed pancreatic surgeries can be of following types:
1: Pancreatoduodenectomy (Whipple’s Procedure): It involves removal (resection) of head of the pancreas along with the duodenum, part of stomach and bile duct and gall bladder. It is performed of cancers in the pancreatic head or lower bile duct, duodenum or ampulla. Continuity of stomach, bile duct and remaining pancreas is restored by reconstruction using small intestine. It is major surgery and involve at least a week of hospital stay. Major complications include leakage from pancreatic reconstruction and delayed gastric emptying (inability to tolerate food temporarily).
2. Distal Pancreatectomy with or without Splenectomy: It involves removal (resection) of body and tail of pancreas. As the spleen is very close to the tail of the pancreas the spleen needs to be removed in some cases. It is required in cases or cancers arising in body and tail portion of pancreas.
3. Total Pancreatectomy: Complete removal of total pancreas.
B. Pancreatic Drainage Procedures: Pancreas is often the site of recurrent infections especially in chronic alcoholics or as a complication of gall bladder stones. Such infections mostly settle down with treatment. However repeated attacks of such infections might cause serious problems (chronic pancreatitis) along with blockade of pancreatic duct with stone formation. This may manifest as severe intractable pain in abdomen and back and require surgical drainage (Pancreaticojejunostomy). Sometimes pancreatic infection can lead to serious complications like pancreatic necrosis or formation or cystic collections (pancreatic pseudocysts). These are life threatening complications and needs surgical intervention (Pancreatic necrosectecomy, Pseudocyst drainage via cystogastrostomy or cystojejunostomy).
1. Pancreatojejunostomy: As mentioned recurrent attacks of pancreatic infections (pancreatitis) can lead to serious hardening of pancreas along with blockade of pancreatic duct with stone formation in the pancreatic channel (duct) causing severe and intractable pain. The surgery involves opening and clearing of pancreatic duct and joining (reconstruction) with small intestine. A part of pancreatic head is might also be removed sometimes.
2. Pancreatic Necrosectomy: In serious pancreatic infections pancreas may be completely damaged and necrosed. This is a very serious condition and may be life-threatening. Surgical removal of infected and necrotic part may be life saving. This surgery might have to be repeated in sessions and single session may not be enough.
3. Cystogastrostomy / Cystojejunostomy: Pseudocysts are fluid filled collections around the pancreas. They are formed as a result of long term complications of severe pancreatic infections. These can grow in size, get infected and cause discomfort and needs treatment. The treatment is to drain them into the bowel either stomach or small intestine depending upon their location and proximity. Cystogastrostomy means drainage into the stomach and cystojejunostomy means drainage into the small intestine.
